24 May Injury Management – Heat Therapy or Ice?
Should I use heat or ice on my injury?
A common question our Physiotherapist’s get asked is whether someone should use heat or ice to treat their injury. The answer to this depends on several factors including the type of injury you have, the mechanism of injury and the length of time you have had the injury. Injuries occur in many ways, more commonly they occur during sporting activities or following trauma like a fall. One of the first things that comes to mind following an injury is to apply heat or ice to the affected area. However in order to understand whether heat or ice would be more beneficial it’s important to understand the difference between acute and chronic injuries.
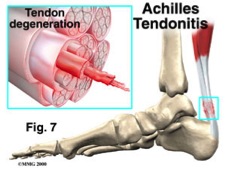
Acute Injuries & Ice:
An acute injury refers to an injury that’s only recently occurred. Injuries like a recent ankle sprain or low back strain are acute and often involve tissue damage and inflammation around the site of injury. Due to the inflammatory process in an acute injury, there is an increase in blood flow to the affected area, resulting in swelling and heat. In these cases applying ICE helps to constrict the blood vessels, slow down the inflammatory process and thus may help to reduce swelling and minimise pain.

In an acute injury it’s important to apply ice sooner rather than later to reduce inflammation and help facilitate healing. At Fleurieu Physiotherapy & Wellness we recommend applying ice to the site of injury for 5-10minutes, then having 20minutes off with no ice. We usually recommend you do this for the first 24-48hours following an acute injury. Leaving ice on the affected area for greater lengths of time has the potential to irritate the skin. If you are not sure whether your injury is improving, it is always best to seek advice from your Fleurieu Physiotherapy & Wellness physiotherapist, as you may need further treatment to assist in your recovery.
Chronic Injuries & Heat:
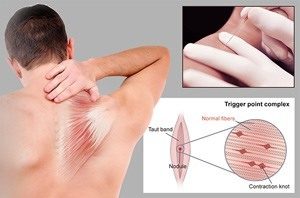
Longstanding injuries or chronic pain conditions generally respond better to HEAT. Chronic pain is classified as pain that has been going on for greater than 3 months, for example recurrent low back pain or stiff, painful knee arthritis. Appling heat to the affected site increases blood flow to the area, stimulating circulation and increasing tissue elasticity. This then helps to facilitate muscle relaxation which may in turn provide pain relief.
Application of heat to an injured or chronically painful area is also useful in managing stress and muscle tension. A common example is people using a heat pack around the base of their neck where the upper trapezius muscles become very tight and sore. At Fleurieu Physiotherapy & Wellness we do not recommend using heat therapy for prolonged periods of time due to the risk of skin irritation or possible burns. Always read the instructions on your heat pack prior to use.
Regardless of the type of injury you have it is always best to seek professional advice if your injury does not improve in a timely manner. Injuries that are not treated properly have the potential to cause recurrent problems and chronic pain, hence it is better to engage in proper rehabilitation early on. At Fleurieu Physiotherapy & Wellness all our physiotherapists are experienced in treating both acute and chronic complaints yielding great relief for our clients. For more information on injury management and how to best treat your injury, call Fleurieu Physiotherapy & Wellness on 85287650 or click the book-online tab.